Triage, is a word derived from the French verb trier, which means to separate, sift or select.
It is really a management process and management consultants constantly use the system to make management systems more efficient.
It can can be applied to any workflow component of a pharmacy, and so the word has slightly different meanings depending on the setting of the triage work flow, and the activity volume and health conditions being experience by the patients that undergo triage.
For example, some pharmacies triage their incoming prescriptions and grade them for order of dispensing and provision of “add-ons” (such as providing CMI or extra reinforcement counselling).
This ensures scarce resources (pharmacist time, assistant back up, knowledge extracts for counselling) can be rationed, but still ensure timely and adequate patient service coverage.
In the UK the Lloydspharmacy group have had a degree of success through positioning pharmacists at a front of shop location, using a bench equipped with wi-fi communications systems, knowledge storage and access systems, and verbal communications systems with key service personnel.
The bench is located at the front of the pharmacy, well clear of the dispensary, ensuring a clear demarcation between the function of a clinical service space compared to that of a dispensary space.
Both are clinical functions, but have work flows that are diametrically opposed.
Click on image below for a larger view.

Triage service provided
These “forward pharmacists” greet patients personally and perform multiple services, (one of which is triage), and refer patients to other health providers external to the pharmacy, or to specialist pharmacists within the pharmacy.
The Pharmaceutical Society of Australia (PSA) have developed research into the positive economic returns by having a “forward pharmacist”.
They have yet to join the dots and determine how to permanently base the forward pharmacist in a clinical space – also the duties of that pharmacist.
Some form of adapted triage would provide a natural “anchor”, allowing other services to be built around that activity.
The term triage may have originated during the Napoleonic Wars from the work of Dominique Jean Larrey.
The term was used further during World War I by French doctors treating the battlefield wounded at the aid stations behind the front.
Those responsible for the removal of the wounded from a battlefield or their care afterwards would divide the victims into three categories:
* Those who are likely to live, regardless of what care they receive;
* Those who are likely to die, regardless of what care they receive;
* Those for whom immediate care might make a positive difference in outcome.
So the triage had its origins among separating the casualties from war as a means of apportioning support services and other aid resources on a rationed basis e.g. doctor, paramedic or nursing human resources, mobile medical vehicle or other patient transport systems in a pre-hospital setting.
Triage also evolved to be applied to other forms of catastrophe (natural disasters, mining accidents etc.).
A tagging system has developed over time to accompany each patient.
As patients are channelled to the ED of a hospital they are processed through a more refined triage process, where the patient’s tag is replaced or updated by the doctors and nursing staff in the ED.
Since the Vietnam war triage processes have moved as close as possible to the battlefront and includes the use of demountable assessment stations and helicopter evacuation processes to create rapid patient clearance.
A triage tag is a prefabricated label placed on each patient that serves to accomplish several objectives:
* identify the patient.
* bear record of assessment findings.
* identify the priority of the patient’s need for medical treatment and transport from the emergency scene.
* track the patients’ progress through the triage process.
* identify additional hazards such as contamination.
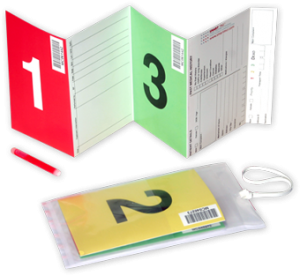
Triage tags may take a variety of forms. Some countries use a nationally standardized triage tag while in other countries, commercially available triage tags are used – and these will vary by jurisdictional choice.
Until recently, Australia used multiple systems within each state (or even within each emergency service within each state).
It has now adopted the system illustrated on a national basis.
The company that developed the tagging system as illustrated (TSG Associates) has partially developed pathways into health systems that pharmacy could adapt for its own purpose.
They even provide online education for different categories of emergency triage.
One new revolutionary addition to the “tagging” process has been to include read/write RFID electronic tags to the hard copy tag, and that has created two positive advantages:
* The patient can be easily found using an electronic reader.
When mass casualties occur (as in war), patients can be tagged immediately with any identifying details, allowing paramedics to move on quickly to process other casualties.
Patients get lost very easily when they all look the same with dressings covering a range of body parts (including the face).
Patient retrieval can then be made electronically, ensuring the most urgent cases are taken first.
* Depending on the range of the RFID tag, forward information can be made available as electronic information is collected by the treatment point before the patient actually arrives.
This allows for staff rostering and drug preparation to commence, again before arrival of the patient.
Looking at pharmacy as a full component of the healthcare system, it does not take too much imagination to envisage:
* 5000 nationally distributed triage points containing clinical pharmacists capable of performing disaster triage including warfare, natural disasters and infection outbreaks at pandemic level.
Given pharmacy moves to establish vaccination clinics, they could prove extremely useful in any pandemic situation as a strategic resource (decentralised locations, stock on hand, trained personnel)
Future planning by government should look at integration of pharmacies within their emergency systems.
In fact, this is an issue that could separate pharmacy from its retail nemesis, having a solid reason for location rules supporting future triage need.
With the range of wars springing up around the world, it is possible that this phenomenon will eventually touch us.
Islamic terrorists and Islamist Indonesia are on our doorstep and the threat potential is real.
Pharmacies/pharmacists ought to be incorporated as part of Australia’s emergency service support because of their strategic locations alone.
i2P has already identified that the new paradigm pharmacy needed to emerge within the coming decade will comprise a multi-story building that contains a range of specialised functions.
One consideration may be a wound dressing facility capable of becoming a patient holding facility for a short time period, in an emergency.
* Looking at the NSW Health policy (which is basically now a national standard and found at Australian Triage) it can be seen that the SMART Tag accredited triage system could have its third channel of priority directed to pharmacists for treatment or other referral.
These are tagged green in the national triage system, as noted below in a policy extract:
3) Third (Delayed) Priority Less serious casualties who do not require treatment within 4-6 hours.
Again, with a bit of imagination, these patients could be further triaged from a pharmacy, particularly one that has a “pharmacy in the home” resource that utilises remote patient monitoring using sensors, notepads and Skype and other communication systems.
It also provides an opportunity for nurse collaboration.
i2P has already planned to integrate this system segment with an existing security services company which has TAFE certificated trained guards in medication administration and who can handle basic first aid.
Using their patrol down time (mostly daylight hours from 5 am to 7 pm) we can provide an economical physical patient monitoring service which can stretch to emergency situations at night.
A visit is activated through a patient button alert or the pharmacist scheduling a periodic “just in case” check.
This does not displace nurses, but ensures the viability of the total service.
Nurses are used when their specialty applies.
And again visualise this entire system as part of a mass casualty triage.
* Remote patient monitoring (RPM) noted above is a technology to enable monitoring of patients outside of conventional clinical settings (e.g. in the home), which may increase access to care and decrease healthcare delivery costs.
The i2P model for “pharmacy in the home” is mainly built around that other area of “mass casualties” and that is the ageing population explosion and chronic illness.
Governments are seemingly well behind in their planning, but getting behind pharmacists for funding remote monitoring services is really a “no brainer”.
Incorporating RPM in chronic disease management can significantly improve an individual’s quality of life.
It allows patients to maintain independence, prevent complications, and minimize personal costs.
RPM facilitates these goals by delivering care right to the home.
In addition, patients and their family members feel comfort knowing that they are being monitored and will be supported if a problem arises.
This is particularly important when patients are managing complex self-care processes such as home hemodialysis.
Key features of RPM, like remote monitoring and trend analysis of physiological parameters, enable early detection of deterioration; thereby, reducing number of emergency department visits, hospitalisations, and duration of hospital stays.
The need for wireless mobility in healthcare facilitates the adoption of RPM both in community and institutional settings is a good investment.
The time saved as a result of RPM implementation increases efficiency, and allows healthcare providers to allocate more time to remotely educate and communicate with patients.
The above facility can double as a mass casualty system, and if it is already in place and tested through chronic illness patients, government can seamlessly advance its security and emergency planning with lower cost, through competent pharmacists with a willingness to co-invest.
But I would add we need to have better support and payment than we have received for managing the PBS.
There are many more positives for consideration:
* An Internet search for Pharmacy Triage yields very little regarding early adopters anywhere in the world except for the UK.
But there is one study in Australia undertaken by three researchers – Professor Colin Chapman, Associate Professor Jennifer Marriott, and Denise van den Bosch,
Funding was provided under the 4CPA in 2009 facilitated by the Pharmacy Guild of Australia with the assistance of 24 Victorian pharmacies.
A paper was published under the title The-Nature-Extent-and-Impact-of-Triage-Provided-By-Community-Pharmacy-in-Victoria-Full-Final-Report- which can be read through the link provided.
It is a quality paper and every pharmacist should read it.
* i2P has been building up a library of its own research and has started releasing this material progressively.
This article is aimed at Pharmacy Leadership organisations, entrepreneurial pharmacists and health departments within the various layers of government.
It provides a practical and economical pathway to harness a resource, much of which has already been performed by pharmacists, but not publicised to any degree.
I have friends who provide consultancies in war zones on a regular basis, helping to set up drug distribution services in war-torn countries and assisting in patient evacuation during major disasters, including warfare.
Most pharmacists provide a form of triage within their pharmacies when referring walk-in patients to other health providers.
That it has not been done efficiently is acknowledged.
That there has been a positive investment in triage research by the PGA is acknowledged.
There is a huge opportunity here for professional development, and the education to back it.
It also requires formal recognition of clinical pharmacists to provide the specialty services.
To the best of my knowledge there has been no attempt to formally link pharmacy into the primary health care system or the emergency care system, even though pharmacists have been involved and at one stage nearly 70 percent of Australia’s primary health care was conducted by pharmacists.
The PBS is considered a primary health care activity by government, but it has become commoditised completely and is now at the end of its product life cycle.
This article provides a suggested outline that would allow pharmacists to fill some gaping “holes” in the health care system at an economical cost.
* And don’t forget professional collaboration.
The above model allows for integration with clinical nurse practitioners, physician assistants and a range of allied health practitioners.
It is a patient-centred system that can fill some gaps in the medical concept of a “patient home”, and it is definitely a patient centred system.
I hope that this article will stimulate our professional leaders to get behind this type of concept or an offshoot stimulated by the content provided.
If anyone wishes to discuss any of the above my email is neilj@computachem.com.au and my telephone contact is
(02) 6628 5138.
